Colorectal cancer, often called colon cancer, is the second leading cause of cancer-related deaths in the United States despite the fact that it is largely preventable.
Colorectal cancer affects both men and women equally, yet awareness regarding its preventability and early detection remains surprisingly low. As a gastroenterology team deeply committed to promoting awareness and understanding of digestive health, we recognize the critical importance of shedding light on this prevalent and potentially life-threatening condition.
 What is Colon Cancer?
What is Colon Cancer?
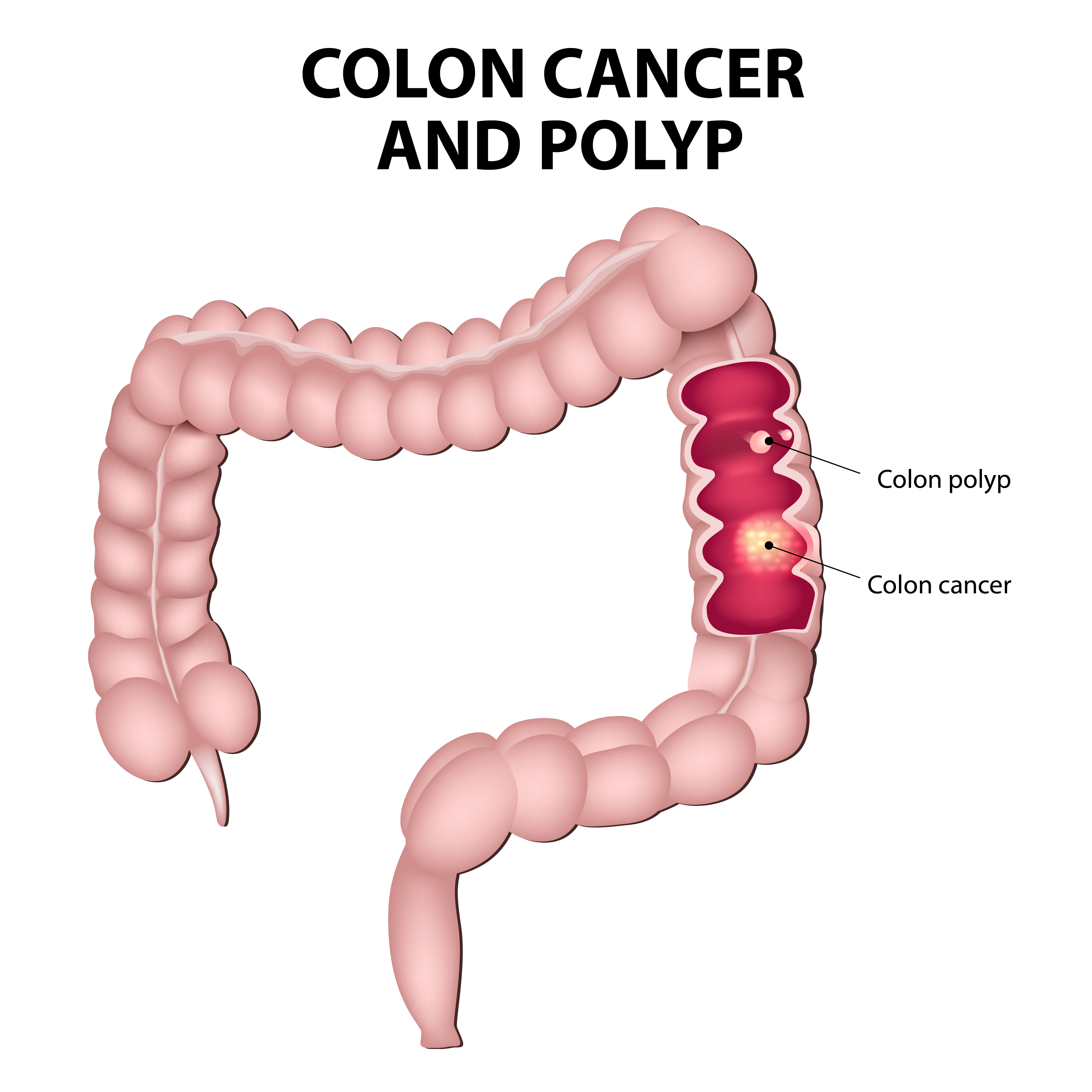
Colon cancer starts in the colon. It usually begins as a small noncancerous growth on the surface of the colon called a colon polyp. Over time, some of these polyps can turn into cancer.
Risk and Causes
Colon cancer is one of the most common cancers worldwide. It affects people of all ages and places. Age is a notable factor, however, with most cases arising in individuals aged 50 and above. Unfortunately, there’s a concerning trend of increasing diagnoses among younger populations since the 1990s, and therefore, experts recommend screening beginning at age 45.
Some people have a higher chance of developing colon cancer. This includes those with family history of colon cancer or colon polyps, a personal history of precancerous colon polyps, African Americans, some Jewish groups, and those with a history of inflammatory bowel diseases such as Crohn’s disease, ulcerative colitis, or hereditary colorectal cancer syndromes, and those with a history of abdominal or pelvic radiation treatment.
We are not sure exactly what causes colon cancer, but certain risk factors are associated with the disease. Lifestyle choices such as diet, tobacco smoking, and excessive alcohol consumption can heighten susceptibility to colorectal cancer. Obesity and genetic factors also play a role in the risk for colon cancer, making clear the importance of preventive measures and early detection.
Treatment Options
Factors including cancer stage, tumor location, and patient health status determine the most effective method of treatment. These treatments can include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy.
Prognosis
Encouragingly, an early-stage colorectal cancer diagnosis often has favorable outcomes, with high survival rates when promptly identified and managed. Cancer found at advanced stages poses greater challenges with less favorable outcomes.
Recognizing Symptoms
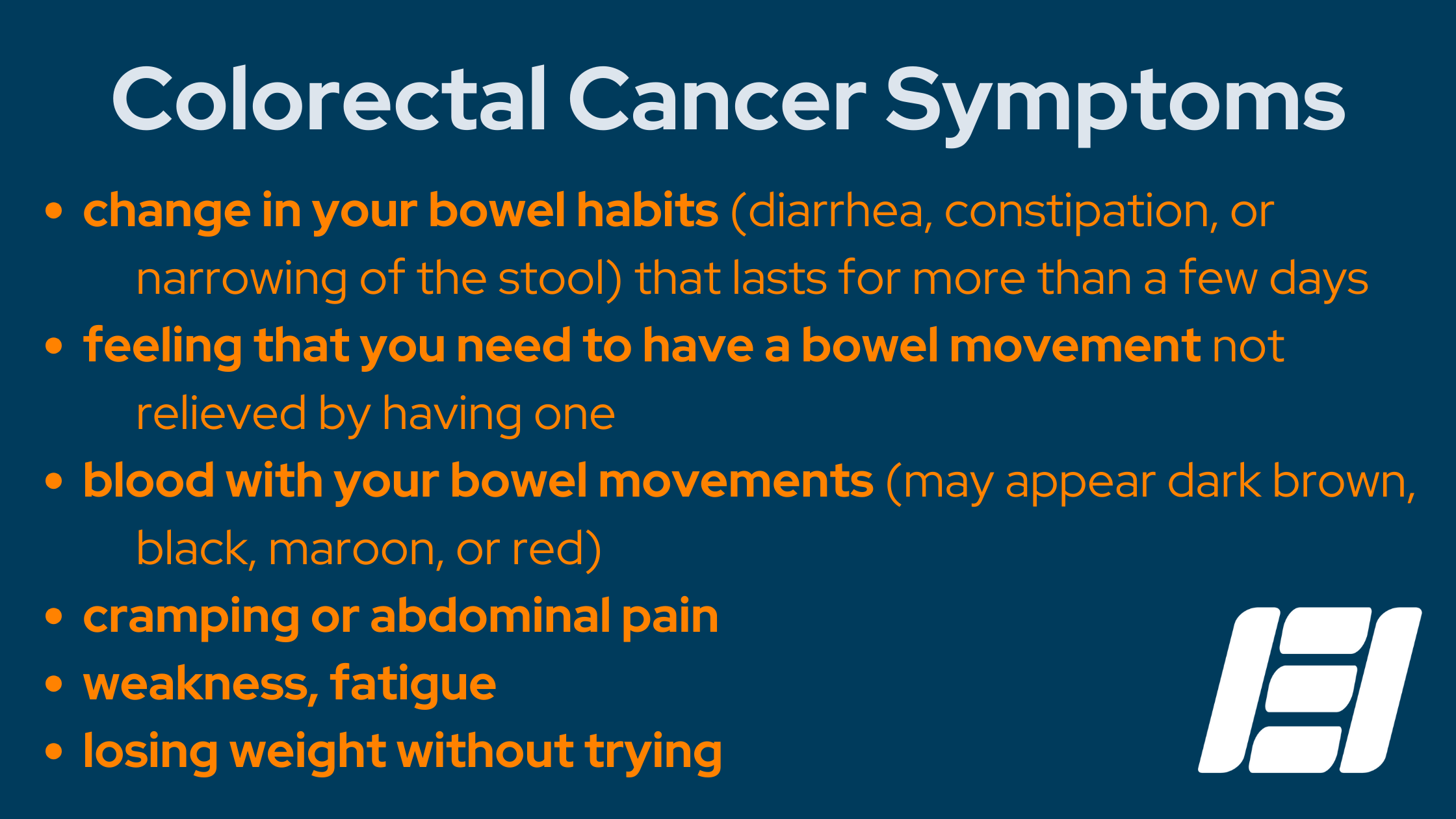
Colon cancer does not always cause symptoms right away. When it does, it can look like other gut problems like infections, hemorrhoids, irritable bowel syndrome, or inflammatory bowel disease. If you notice any of these symptoms, see your doctor right away.
Screening Options
For individuals at average risk, screening should begin at age 45. However, those at increased or high risk, such as those with a family history of colon cancer or certain genetic conditions, may need to start screening earlier, undergo more frequent screening, and possibly require specialized tests.
Now, let’s delve into the various screening methods available for colorectal cancer:
1. Colonoscopy
This gold-standard screening tool involves a thorough examination of the entire colon using a flexible, illuminated tube equipped with a camera. During the procedure, patients receive medication to induce relaxation and comfort. If polyps are discovered, they can be removed on the spot, potentially avoiding the progression to cancer. A thoroughly pre-cleansed colon ensures the best visualization and increases the likelihood of detecting and removing polyps, so some preparation is required before a colonoscopy. Following the procedure, patients require a companion to accompany them home, and if no abnormalities are found, a repeat colonoscopy is typically scheduled in 10 years for average-risk individuals.
2. Stool DNA Test (Cologuard)
Unlike colonoscopy, this non-invasive test analyzes stool samples for DNA changes indicative of colon cancer. It can be performed at home without any preparation. However, it is less effective at detecting precancerous polyps and may yield false-positive results, necessitating follow-up with a colonoscopy.
3. Fecal Occult Blood Test (FOBT)
FOBT involves testing stool samples for hidden blood, which can signal the presence of certain abnormalities and can yield false-positive results due to dietary or medication influences.
Selecting the most appropriate screening method hinges upon individual risk factors, preferences, and health care provider guidance. We urge you to engage in open dialogue with your primary care physician to navigate these options.
Colorectal cancer screening is a critical tool in fighting colon cancer and maintaining overall health. As advocates for digestive health and proactive health care, the team at Elliot Gastroenterology remains steadfast in our commitment to combating colorectal cancer. Through education, vigilant screening initiatives, and personalized treatment plans, we look towards a future where colorectal cancer is significantly reduced and for the most part, prevented.
Learn more about colorectal cancer screening and Elliot Gastroenterology

By Dr. Arathi Komarla, Nicole Jimenez, APRN, and Brittany Boutin, RN of Elliot Gastroenterology
